Anorexia Nervosa Uncovered
[TRIGGER WARNING: The article below mentions eating disorders. Reader discretion is advised.]
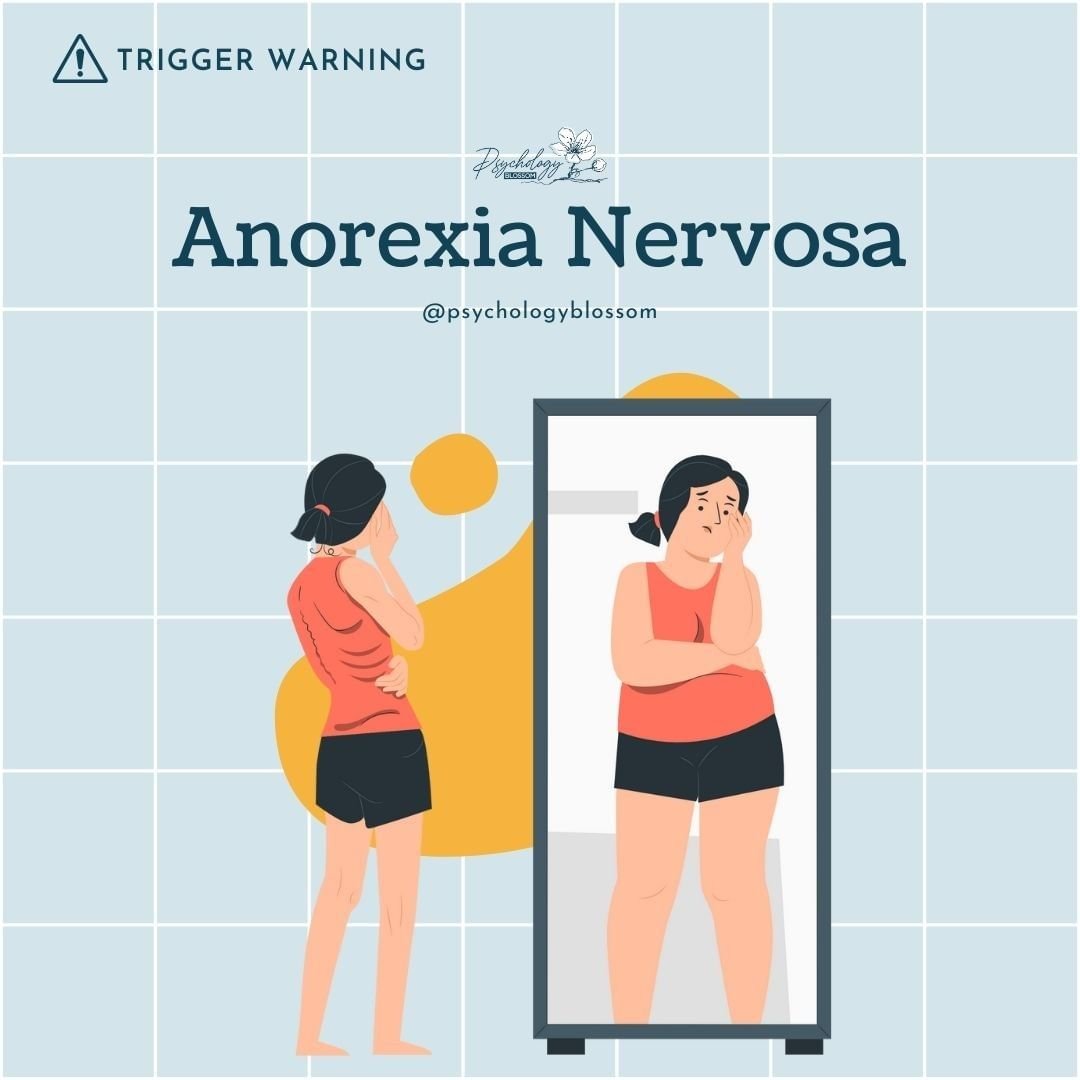
Anorexia Nervosa, or anorexia, is an eating disorder which involves the partial or total abstinence from food (solids or liquids) because one believes any amount of food will cause weight gain. A person with anorexia often perceives herself/himself as ‘fat’ and has an intense fear of gaining weight.
To prevent weight gain or to continue losing weight, people with anorexia usually severely restrict the amount of food they eat. They may control calorie intake by vomiting after eating or by misusing laxatives, diet aids, diuretics or enemas. They may also try to lose weight by exercising excessively. No matter how much weight is lost, the person continues to fear weight gain.
Anorexia isn’t really about food. It’s an extremely unhealthy and sometimes life-threatening way to try to cope with emotional problems. When one has anorexia, they often equate thinness with self-worth. Over time, preoccupation with weight and shape can dominate thinking, crowding out relationships, hobbies, and academic or work goals.
Symptoms
The physical signs and symptoms of anorexia are related to starvation. Anorexia also includes emotional and behavioral issues involving an unrealistic perception of body weight and an extremely strong fear of gaining weight or becoming fat.
It may be difficult to notice signs and symptoms because what is considered a low body weight is different for each person, and some individuals may not appear extremely thin. Also, people with anorexia often disguise their thinness, eating habits or physical problems.
✽ Physical Signs May Include:
- Extreme Weight Loss
- Thin Appearance
- Fatigue
- Insomnia
- Dizziness or Fainting
- Bluish Discolouration of the Fingers
- Hair that Thins, Breaks or Falls Out
- Absence of Menstruation
- Constipation and Abdominal Pain
- Dry or Yellowish Skin
- Irregular Heart Rhythms
- Dehydration
- Swelling of Arms or Legs
✽ Behavioural Symptoms May Include Attempts to Lose Weight by:
- Exercising excessively
- Frequently skipping meals or refusing to eat
- Denial of hunger or making excuses for not eating
- Eating only a few certain “safe” foods, usually those low in fat and calories
- Not wanting to eat in public
- Lying about how much food has been eaten
- Repeated weighing or measuring the body
- Frequent checking in the mirror for perceived flaws
- Complaining about being fat or having parts of the body that are fat
- Covering up in layers of clothing
Complications and Medical Risks
Without timely support, anorexia can lead to serious complications: electrolyte imbalances, low blood pressure, heart rhythm abnormalities, bone mineral loss (osteopenia/osteoporosis), anemia, immune suppression, infertility, and organ strain. In severe cases, it can be fatal. Medical monitoring is therefore a vital part of treatment to ensure safety during weight restoration and recovery.
Causes
The exact cause of anorexia is unknown. As with many diseases, it’s probably a combination of biological, psychological and environmental factors.
✽ Biological
Although it’s not yet clear which genes are involved, there may be genetic changes that make some people at higher risk of developing anorexia. Some people may have a genetic tendency toward perfectionism, sensitivity and perseverance — all traits associated with anorexia. Neurobiological factors (e.g., how the brain processes reward and anxiety) may also play a role.
✽ Psychological
Some people with anorexia may have personality traits that make it easier to stick to strict diets and forgo food despite being hungry. They may have an extreme drive for perfectionism, which causes them to think they’re never thin enough. And they may have high levels of anxiety and engage in restrictive eating to reduce it. Low self-esteem, harsh self-criticism, and black-and-white thinking are common.
✽ Environmental
Modern Western culture emphasizes thinness. Success and worth are often equated with being thin. Peer pressure may help fuel the desire to be thin, particularly among young girls. Social media comparison, participation in appearance-focused activities (e.g., certain sports, dance), and weight-based comments can increase vulnerability.
Risk Factors
✽ Gender
Anorexia is more common in girls and women. However, boys and men have increasingly developed eating disorders, possibly related to growing social pressures. People of any gender identity can be affected.
✽ Age
Anorexia is also more common among teenagers. Still, people of any age can develop this eating disorder, though it’s rare in those over 40. Teens may be more at risk because of all the changes their bodies go through during puberty. They may also face increased peer pressure and be more sensitive to criticism or even casual comments about weight or body shape.
✽ Genetics
Changes in specific genes may put certain people at higher risk of anorexia. Those with a first-degree relative — a parent, sibling or child — who had the disorder have a much higher risk of anorexia.
✽ Dieting
Dieting is a risk factor for developing an eating disorder. There is strong evidence that many of the symptoms of anorexia are actually symptoms of starvation. Starvation affects the brain and influences mood changes, rigidity in thinking, anxiety and reduction in appetite. Starvation and weight loss may change the way the brain works in vulnerable individuals, which may perpetuate restrictive eating behaviours and make it difficult to return to normal eating habits.
✽ Transitions
Whether it’s a new school, home or job; a relationship breakup; or the death or illness of a loved one, change can bring emotional stress and increase the risk of anorexia.
How Anorexia is Diagnosed
A licensed clinician will assess medical status, weight history, eating patterns, exercise, thoughts and emotions related to food and body image, as well as social and family context. Laboratory tests and ECG may be ordered to evaluate complications. Diagnosis considers the severity of restriction, fear of weight gain, and body image disturbance—not just appearance.
Treatment
A healthcare professional will make a comprehensive plan to address the individual’s specific needs. It will involve a team of specialists who can help the person overcome the physical, emotional, social, and psychological challenges that they face.
Strategies include:
- Cognitive-Behavioural Therapy (CBT), which can help the person find new ways of thinking, behaving, and managing stress
- Family and Individual Counselling
- Nutritional therapy, which provides information on how to use food to build and maintain health
- Supplements to resolve nutritional deficiencies
Additional evidence-based approaches include Family-Based Treatment (FBT) for adolescents, which empowers caregivers to support re-feeding and disrupt disordered behaviors; and therapies like MANTRA or ACT in certain cases. Medical care may address complications, guide safe weight restoration, and monitor for refeeding syndrome. Levels of care range from outpatient to day programs, residential, or inpatient treatment depending on medical and psychological risk.
Motivation, Ambivalence, and Relapse Prevention
Engaging in treatment can be challenging because the illness often convinces the person that maintaining low weight is necessary. Motivation can fluctuate; this is normal and workable. Relapses can occur, especially during the first 2 years. A relapse-prevention plan might include regular meals and snacks, clear support contacts, scheduled medical/therapy follow-ups, and early-warning signs (e.g., renewed calorie counting, body checking, isolation). Family and friends can provide crucial support by learning about the condition, using non-judgmental language, and focusing on health and values beyond weight or appearance.
Helping a Loved One
If you’re worried about someone, choose a calm, private time to share observations (“I’ve noticed you seem tired and skipping meals”) rather than judgments. Offer to help them find support and accompany them to appointments. Avoid diet talk or body comparisons. Celebrate steps toward recovery unrelated to weight: flexibility, social connection, and self-care.
Self-Care and Everyday Supports
Recovery grows from many small actions repeated over time. Gentle structure helps: three meals and two to three snacks daily; scheduled rests; limiting compulsive exercise until cleared by a clinician; and practicing skills for anxiety and perfectionism. Building a compassionate inner voice, reconnecting with enjoyable activities, and setting boundaries with triggering media or conversations can protect progress.
When to Seek Urgent Help
Seek immediate medical attention if there is fainting, chest pain, a very low heart rate, vomiting multiple times a day, blood in vomit, severe dehydration, or inability to keep food/fluids down. If there are thoughts of self-harm or suicide, contact emergency services or a crisis line right away.
We recommend This Video to those who wants to learn more about Anorexia Nervosa.
About Us
We are a team comprising psychologists based in Singapore endeavouring our best to prioritise our clients’ needs. When you embark on this journey with us, we take a collaborative approach where you and your psychologist work closely together, and listen to what you have to say — No judgments, and in a safe space. Meet our Team
Quick Links
Contact Us
150 Cecil Street #07-02 S069543
Opening Hours
Monday to Friday: 8am to 6pm
Saturday: 8am to 2pm
Sunday: 10am to 2pm (Online only)
Admin Hours
Monday to Friday: 8am to 5.30pm
Saturday: 8am to 2pm
© Copyright 2023 – Psychology Blossom | Privacy Policy | Terms