Everyone Deserves To Blossom
Nunc tincidunt egestas velit nec efficitur. Duis vestibulum volutpat nibh sed consequat. Maecenas tincidunt, arcu vel iaculis cursus.
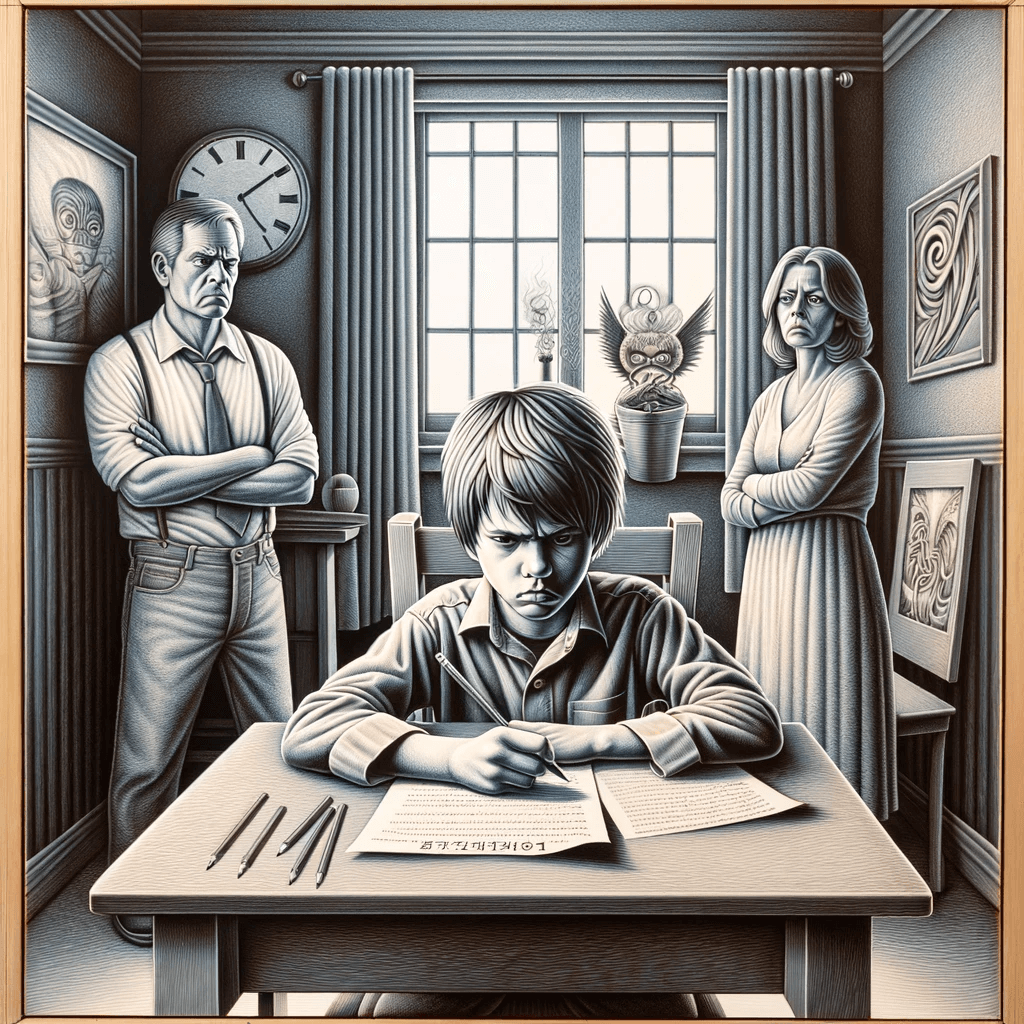
Even the most well-behaved children may be difficult and challenging at times. In fact, at certain developmental stages, it would be unusual if they do not throw any tantrums or meltdowns. Oftentimes, small amounts of this constitute a healthy and essential part of growing up.
However, if there is a frequent and persistent pattern of anger, irritability, arguing, defiance, or vindictiveness towards parents or other authority figures, which is age-inappropriate, this may indicate Oppositional Defiant Disorder (ODD).
To help you better understand this mental health disorder, this post includes the following information:
Oppositional Defiant Disorder is a behaviour disorder in which children display consistent patterns of hostility, disobedience, and defiance towards family, peers, or other authority figures. Although it’s common to see children defying authority once in a while, children with ODD do it more frequently and with more hostility than their peers. If this behaviour persists for more than 6 months and goes beyond the typical behaviour of your child’s age, then it might be an indicator of ODD.
Research studies suggest that oppositional defiant disorder affects 2-11% of children. This variation is due to underdiagnosis or misdiagnosis as conduct disorder (CD). Moreover, it is rarely diagnosed in older children or adolescents because symptoms of ODD might get misunderstood as typical teenage behaviour. However, it’s important to note that the prevalence of ODD declines with increasing age.
Children and teenagers diagnosed with the following mental health conditions are more prone to development of Oppositional Defiant Disorder:
Additionally, research studies indicate individuals who have experienced ODD have a 92.4% chance of meeting the criteria for at least one of the disorders outlined in DSM-IV. It includes disorders related to mood (45.8%), anxiety (62.3%), impulse control (68.2%), and substance use (47.2%).
Usually, signs and symptoms of Oppositional Defiant Disorder are evident during preschool years and can act as a precursor to Conduct Disorder (CD). These signs remain relatively stable between the ages of 5 and 10, but their prevalence declines afterwards. Nonetheless, differentiating between a strong-willed child and one displaying signs of this disorder can be challenging.
We can further categorise the signs of ODD into three distinct parts:
Symptoms include:
Oppositional Defiant Disorder can be mild, moderate, or severe. Initially, symptoms may become apparent only at home. But as the condition worsens, it may manifest in other settings, such as at school, work, or with peers.
Symptoms appear only in one setting.
Symptoms appear in at least two settings.
Symptoms appear in three or more settings.
The exact cause is complex and often results from a combination of the following factors.
Children who have other mental health conditions, such as ADHD, Bipolar Disorder, Mood Disorder, or Anxiety Disorder, are also at the highest risk for ODD.
Children whose parents suffer from ODD are at the highest risk of developing it. Furthermore, if they have close family members with mental illnesses, such as mood disorders, anxiety disorders, or learning disabilities, they are more likely to develop Oppositional Defiant Disorder. It shows the interlinking between mental health conditions and genetics.
The environment in which a child grows up significantly influences whether or not they develop this condition. An example of an environment that may lead to the development of ODD includes:
ODD is associated with an imbalance in brain chemicals, such as serotonin. These chemicals, known as neurotransmitters, are important in facilitating communication between nerve cells. Therefore, an imbalance in neurotransmitters can affect reasoning, judgement, and impulse control.
Some of the risk factors associated with the development of ODD include:
Kids who have difficulty managing their emotions are prone to the development of Oppositional Defiant Disorder.
Dysfunctional family life, absolute neglect, abuse, inconsistent discipline, or substance abuse.
Parents who have had ODD or other mental health conditions like mood disorder, anxiety disorder, or learning disability might increase the likelihood of their children getting it.
Attention or rejection from a peer might contribute to these behaviours.
While prevention might not always be possible, early detection and treatment at the first sign might improve behaviour and prevent symptoms from worsening. Providing a supportive and nurturing environment at home reduces the distress caused by symptoms and prevents defiant behaviours. Moreover, early treatment may build self-esteem and relationships with those around them. The sooner individuals receive the necessary treatment, the better the outcomes.
Since there is no specific test, medical healthcare providers conduct a series of detailed assessments to evaluate ODD.
The medical diagnosis process includes:
To be diagnosed, your child needs to meet four or more symptom criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) for at least six months. These symptoms must be severe and disruptive, demonstrating the pattern of angry or irritable mood, argumentative or defiant behaviour, or vindictiveness.
Diagnosis involves a detailed psychiatric evaluation of the child with their parents or other authority figures in multiple settings.
Academic and intelligence testing help determine if they have learning disabilities or intellectual problems.
For instance, risk factors such as bullying, abuse, or negligence might contribute to oppositional behaviours. So, it’s incredibly important to identify the risk factors.
ODD often comes with other mental health conditions, making it tricky to separate its symptoms from those of other issues. Improving these symptoms can be tough without addressing the coexisting conditions. That’s why medical professionals need to diagnose and treat any other issues that might be there.
It’s challenging to differentiate this disorder from the other disorders due to its overlapping symptoms. However, distinguishing them from each other is necessary for accurate diagnosis and effective treatment.
Both CD and ODD exhibit similar patterns of disruptive and defiant behaviour. However, CD is more severe and involves issues related to animal cruelty, destruction of property, physical aggression, theft, or serious violation of rules.
ADHD and Oppositional Defiant Disorder often co-exist, and both can manifest as inattention, hyperactivity, and impulsivity. However, ODD primarily involves defiant and oppositional behaviours directed toward authority figures. In contrast, ADHD deals with the inability to focus, impulse control, and fidgety behaviour, often impacting their daily routine.
ODD is often co-morbid with a mood disorder, sharing overlapping symptoms of emotional dysregulation and irritability. However, argumentative, defiant, and vindictive behaviour that occurs in Oppositional Defiant Disorder doesn’t routinely happen in mood disorders. In addition, individuals shouldn’t be diagnosed with it if oppositional symptoms arise only when they are experiencing a mood disorder.
Both DMDD and ODD share symptoms of frequent anger outbursts and irritable moods. However, in DMDD, the irritability moods between the outbursts and the severity of temper outbursts are more intense than in Oppositional Defiant Disorder. Moreover, as per DSM-5, if an individual meets the criteria for both disorders, clinicians should only assign the diagnosis of DMDD.
The treatment plan depends on many factors, such as:
Some of the treatments include:
It is a form of family therapy during which parents acquire skills and techniques from a therapist to navigate and address their child’s behaviour effectively. This approach empowers parents to handle their child’s behaviour simply by reinforcing good behaviour and discouraging bad behaviour. For instance, you can encourage good behaviour by rewarding and praising them.
Research studies suggest that PCIT results in a significant reduction in behavioural problems and an improvement in parents’ parenting skills. It involves real-time coaching sessions where parents learn how to interact with their children. Generally, the therapist sits behind a one-way mirror and guides parents through strategies that reinforce positive behaviour, using a transmitter and receiver system.
PSST is a cognitive-behavioural approach that teaches children techniques for dealing constructively with their thoughts and feelings rather than resorting to dysfunctional ways. This design helps children manage their anger and impulses while generating multiple solutions to their problems.
A child may benefit from social skills training as it helps develop better social and interpersonal skills, which improves peer relationships.
Psychosocial interventions like training or therapy are the first line of treatment for children with ODD. In general, healthcare professionals reserve medications for aggressive and disruptive behaviours that psychosocial intervention alone cannot manage. Although the FDA has not approved any medication for Oppositional Defiant Disorder, in severe cases, they might prescribe atypical antipsychotics like Risperidone or Ariprazole.
If your child is diagnosed with this disorder, aside from getting professional help, you can help your child and yourself by learning various coping skills.
Some of the coping strategies for children and parents include:
Shower them with praises and positive reinforcements when they are on their best behaviour.
When dealing with an ODD child, it’s important to speak calmly. Acknowledge their behaviour and, if necessary, step away from the argument. Removing yourself from the situation takes away the power to control the exchange.
Set a limit or boundary for bad behaviour and enforce it consistently by giving consequences and holding the child accountable for their actions.
Don’t react to everything your child does; stay as neutral and objective as possible. Remember, it’s not about you; it’s about your child and what they need to learn. Try to practice calm and consistent parenting and understand what’s driving your child’s behaviour.
Feeling worn out while dealing with a child who thrives on chaos is normal. Often, parents give in because it’s too overwhelming and exhausting. Therefore, it’s essential to prioritise your physical and mental well-being while also seeking help or support if necessary.
Here are some tips before you get an appointment.
i. Make a list of symptoms your child has been experiencing. It includes:
ii. Gather relevant information. It includes:
iii. Note down questions you might have for your therapist.
iv. Bring a friend or family member for emotional support.

At Psychology Blossom, a Therapy and Counselling Centre based in Singapore, we understand it’s overwhelming and exhausting to deal with a child with Oppositional Defiant Disorder. Our team of experienced psychologists and counsellors in Singapore are here to support you in improving your child’s well-being. Together, we’ll unravel complexities hindering your child’s well-being in our judgement-free, safe space. Remember, consistent support and intervention can make a meaningful difference in your child’s journey towards improved well-being.
ODD can act as a disruptive force, significantly impacting a child’s family or school life. Yet, proactively taking steps like seeking help from a mental health professional acts as an early intervention strategy to improve your child’s behaviour and prevent it from further worsening. Therefore, an effective treatment restores your child’s self-esteem and helps build positive relationships with those around them.