Borderline Personality Disorder (BPD): Signs, Types, Causes, and Treatment

Individuals with Borderline Personality Disorder (BPD) display a pattern of behaviour involving impulsivity and instability in their interpersonal relationships, moods and self-image. Their relationships with others are usually intense but can be stormy and may include over-idealisation of friends, lovers or even therapists. Sometimes these relationships are delusional and result in disappointment or anger that triggers their shift in mood from intense feelings of joy to rage. The opposite is also possible in other situations.
What is Borderline Personality Disorder?
Borderline Personality Disorder (BPD), also known as Emotionally Unstable Personality Disorder (EUPD), is a mental health condition distinguished by a long-term pattern of severe and inconsistent interpersonal relationships, mood swings, deformed self-image, and bumpy emotional responses. It is a serious chronic psychological condition that affects a person’s mood, behaviour, self-image, and relationships. Often, individuals with this condition experience potent and sudden shifts in emotions, impulsive behaviour, and difficulty in sustaining well-balanced relationships. BPD symptoms can be overwhelming and can notably impact a person’s daily life at home, work, and in the community.
Some common BPD traits include intense fear of rejection, depressed mood, self-harm tendencies, chronic feelings of emptiness, and suicide tendencies. BPD episodes can be stimulated by undesirable events or perceived rejection, leading to vehement mood swings, anger, and recklessness. Mental health professionals usually diagnose it by thoroughly evaluating the individual’s symptoms and medical history.
While there is no known panacea for BPD, focused treatment can help affected individuals manage their symptoms and improve their quality of life. For those seeking information, it’s necessary to recognise the importance of early diagnosis and intervention. Treatment options may include talk therapy, dialectical behaviour therapy (DBT), cognitive-behavioural therapy (CBT), medication, and lifestyle changes. Appropriate treatment aims to help individuals manage negative emotions, learn healthier coping skills, and build more stable relationships.
Examples of the “all-or-nothing” swings someone may notice include:
- “My life is going great” VS “Nothing is working out, I’m going to fail regardless.”
- “Our relationship is perfect; he will love me forever” VS “He hates me; he is going to leave me.”
Types of Borderline Personality Disorder
Officially, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) does not recognise specific subtypes for Borderline Personality Disorder. Nevertheless, certain experts propose categorisation into four distinct types, delineated by their predominant symptomatic profiles:
1. Discouraged borderline
A pervasive pattern of hopelessness, low self-esteem, persistent discouragement, and self-criticism. People may struggle with chronic shame, guilt, withdrawal, and a strong need for reassurance.
2. Impulsive borderline
Marked by risk-taking behaviours such as substance misuse, self-harm, reckless spending, binge eating, unsafe sex, and rash driving. Impulsivity can hinder stable relationships and the ability to cope with daily challenges.
3. Petulant borderline
Involves irritability, anger, and impatience. Individuals may come across as bitter and quarrelsome, with temper outbursts, difficulty controlling emotions, and chronic boredom or dissatisfaction.
4. Self-destructive borderline
Characterised by self-harm, suicidal thoughts, and profound emptiness. Intense emotional distress may lead to substance abuse and reckless behaviours, accompanied by feelings of worthlessness and hopelessness.
BPD varies in severity. Therapy (like DBT) and, at times, medication can help manage symptoms. For accurate diagnosis and effective treatment, seek professional help.
Signs and Symptoms of Borderline Personality Disorder (BPD)
Recognising signs early supports understanding and compassionate responses. Common features include:
1. Fear of abandonment
A profound dread of being left, even when the likelihood is minimal, leading to frantic efforts to avoid real or imagined abandonment.
2. Intense and unstable relationships
Rapid shifts between idealising and devaluing others (“splitting”), creating cycles of closeness and conflict.
3. Unclear or shifting self-image (identity disturbance)
Unstable sense of self, frequent changes in values, goals, appearance, or peer group; feeling unsure who you are.
4. Impulsive, self-destructive behaviours
Acting on urges in ways that create harm or regret (e.g., substance misuse, risky driving, binge behaviours).
5. Suicidal thoughts and self-harming behaviours
Using self-injury (e.g., cutting, burning) to cope with emotional pain; recurring thoughts of suicide require urgent professional attention.
6. Extreme mood swings
Sudden, intense shifts such as anger, fear, anxiety, sadness, or euphoria that may last hours to a day.
7. Chronic feelings of emptiness
Persistent inner void, boredom, or a sense that “something is missing,” often tied to low self-worth.
8. Inappropriate or uncontrollable anger
Difficulty regulating anger; outbursts may include shouting, sarcasm, or aggression, followed by remorse.
9. Dissociation or transient paranoia
Feeling detached from self or surroundings; stress-related suspiciousness or perceptual distortions.
Causes of Borderline Personality Disorder
No single cause explains BPD. Most research points to a combination of genetic vulnerability, environmental experiences, and brain-based differences in emotion regulation. The condition may run in families, suggesting heritable risk. Neurobiological studies point to differences in regions involved in impulse control and processing threats or emotions.
Early life experiences can strongly influence development. Adverse childhood events—such as neglect, emotional or physical abuse, or inconsistent caregiving—may heighten risk. Protective relationships, on the other hand, can promote resilience. Understanding the links between genetics, brain function, and early experiences helps tailor interventions and highlights the value of trauma-informed therapy.
Risk Factors of Borderline Personality Disorder
Having risk factors does not guarantee BPD, but it may increase likelihood:
1. Genetics, brain structure, and function
i. Family history
Those with a family history of Borderline Personality Disorder (BPD) have a higher risk.
ii. Brain structure differences
Differences in networks responsible for emotion processing and impulse control may contribute to symptoms.
2. Environment
i. Parenting factors
Adverse experiences such as abuse, neglect, or abandonment—especially when chronic—raise risk.
ii. Cultural influences
Beliefs about emotions, stigma, facial-expression interpretation, and resource access may shape symptom expression and help-seeking.
iii. Social factors
Stressors such as poverty, family disruptions (e.g., parental separation), and community instability can compound vulnerability.
Impact of Borderline Personality Disorder
1. Daily life and relationships
Intense emotions and fear of abandonment can lead to arguments, pushing people away, or clinging; building secure bonds takes time and skills practice. Self-perception may feel unstable, creating confusion about identity, goals, and purpose.
2. Work and social interactions
Mood reactivity and interpersonal sensitivity may complicate teamwork, feedback, and consistency. Without support, people may withdraw or experience frequent conflicts; with treatment and accommodations, many thrive at work and socially.
Borderline Personality Disorder Diagnosis
Assessment by a qualified professional (psychologist or psychiatrist) is essential. Diagnosis considers history, current symptoms, and how long they have persisted. It often includes:
- Clinical evaluation with structured or semi-structured interviews.
- Ruling out other conditions (for accurate diagnosis).
- Collecting collateral information (with consent) from family or friends.
- Determining duration, severity, and pervasiveness of symptoms across settings.
BPD is diagnosed using DSM-5 criteria—identifying a pattern of instability in relationships, self-image, and affect, plus impulsivity. Because BPD often co-occurs with anxiety disorders, bipolar disorder, depression, eating disorders, post-traumatic stress disorder, and substance use disorders, careful differential diagnosis is vital.
Treatment and Management
Effective care is collaborative and holistic—addressing emotions, thinking patterns, behaviour, and the social environment.
1. Psychotherapy
Therapy is the cornerstone of treatment:
i. Dialectical Behavioural Therapy (DBT)
Builds skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness; reduces crises and improves stability.
ii. Cognitive Behavioural Therapy (CBT)
Targets unhelpful thoughts and behaviours; challenges core beliefs (e.g., “I will always be abandoned”) and builds balanced coping.
iii. Schema Focused Therapy
Identifies and transforms long-standing patterns (schemas) developed in childhood that drive current difficulties.
iv. Mentalisation Based Therapy (MBT)
Strengthens the ability to understand mental states in self and others, improving empathy and relationship stability.
v. Systems Training for Emotional Predictability and Problem-Solving (STEPPS)
Group-based program integrating emotion education, problem-solving, and social support to enhance day-to-day functioning.
vi. Transference-Focused Psychotherapy (TFP)
Explores how past relational patterns play out with the therapist to foster insight and healthier attachments.
2. Medication
No medication “cures” BPD, but targeted prescriptions can reduce co-occurring symptoms. Antidepressants may support mood and anxiety; mood stabilisers can help with impulsivity and affective swings; low-dose antipsychotics may reduce cognitive-perceptual symptoms. Medication works best alongside psychotherapy.
3. Prevention and early intervention
Early recognition, psychoeducation, and skill-building reduce crisis frequency and improve long-term outcomes. School and family programs that teach emotion skills and safe relationships can be protective.
4. Support for caregivers and family
Family education, boundary-setting, and communication coaching reduce conflict and burnout. Caregivers benefit from learning validation skills and crisis plans.
What Does Untreated BPD Look Like?
Without support, people may experience unstable relationships, fear of abandonment, impulsive and risky behaviour, extreme mood swings, identity disturbance, paranoia or dissociation, chronic emptiness, self-harm or suicidal thoughts, difficulty controlling anger, and “splitting” between idealising and devaluing others. Timely care can significantly change this trajectory.
Special Considerations
1. BPD in men and women
Presentation may differ by gender and culture; stigma can delay help-seeking. Education and awareness reduce barriers to care.
2. Silent and mild BPD
Some people mask distress or experience subtler symptoms—still worthy of support and treatment.
3. Supporting someone with BPD
Create safety, listen actively, validate emotions, encourage professional help, and set clear, respectful boundaries.
Living with Borderline Personality Disorder
1. Seeking professional help
Qualified clinicians can diagnose, tailor treatment, and coach skills for long-term well-being.
2. Self-help strategies and lifestyle adjustments
- Practising mindfulness and grounding techniques.
- Regular exercise and restorative sleep.
- Balanced nutrition; consistent routines.
- Avoiding drugs and alcohol; limiting triggers where possible.
3. Developing a crisis plan
List early warning signs, coping steps, helpful contacts, and emergency numbers; share with trusted supporters.
4. Building support networks
Peer groups, family, friends, and online communities can provide connection, accountability, and hope.
Research and Future Directions
Current BPD research
Scientists study neurobiology, genetics, and the impact of childhood trauma; neuroimaging helps map emotion and control circuits to refine therapies.
Future trends
Personalised care, digital tools (e.g., skills apps), and precision psychiatry aim to make treatment more accessible and effective.
Get Support at Psychology Blossom for BPD

If you’re fighting with BPD, you’re not alone; Psychology Blossom, a Therapy and Counselling Centre based in Singapore, is here to support you. Our psychologists are trained in evidence-based approaches like Cognitive Behavioural Therapy (CBT) and can help you regulate emotions, strengthen relationships, and build a secure sense of self. To book an appointment with us, contact us at +65 8800 0554.
Conclusion
Borderline Personality Disorder is treatable. With timely intervention, structured therapy, supportive relationships, and practical skills, many people experience meaningful improvement. Recovery is a journey—one worth taking with the right guidance and compassion.
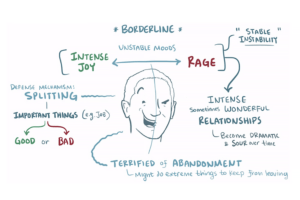
Image Credits: Suendermann, 2019
We recommend This Video to those who wants to learn more about Borderline Personality Disorder (BPD).