Everyone Deserves To Blossom
Nunc tincidunt egestas velit nec efficitur. Duis vestibulum volutpat nibh sed consequat. Maecenas tincidunt, arcu vel iaculis cursus.

Individuals with Borderline Personality Disorder (BPD) display a pattern of behaviour involving impulsivity and instability in their interpersonal relationships, moods and self-image.
Their relationships with others are usually intense but can be stormy and may include over-idealisation of friends, lovers or even therapists. Sometimes these relationships are delusional and result in disappointment or anger that triggers their shift in mood from intense feelings of joy to rage. The opposite is also possible in other situations.
Borderline personality disorder (BPD), also known as Emotionally Unstable Personality Disorder (EUPD), is a mental health condition distinguished by a long-term pattern of severe and inconsistent interpersonal relationships, mood swings, deformed self-image, and bumpy emotional responses.
It is a serious chronic psychological condition that affects a person’s mood, behaviour, self-image, and interpersonal relationships. Often, individuals with this condition experience potent and sudden shifts in emotions, impulsive behaviour, and difficulty in sustaining well-balanced relationships. BPD symptoms can be awful and can notably impact a person’s daily life.
Some common BPD traits include intense fear of rejection, depressed mood, self-harm tendencies, chronic feelings of emptiness, and suicide tendencies. BPD episodes can be stimulated by undesirable events or perceived rejection, leading to vehement mood swings, anger, and recklessness. Mental health professionals usually diagnose it by thoroughly evaluating the individual’s symptoms and medical history.
While there is no known panacea for BPD, Borderline Personality Disorder Therapy can help affected individuals manage their symptoms and improve their quality of life. For those seeking information, it’s necessary to recognise the importance of early diagnosis and conciliation. Treatment options may include talk therapy, dialectical behaviour therapy (DBT), cognitive-behavioural therapy (CBT), medication, and lifestyle changes. Appropriate treatment aims to help individuals manage negative emotions, learn healthier coping skills, and build more stable relationships.
Some examples are:
Officially, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) does not recognise specific subtypes for Borderline Personality Disorder. Nevertheless, certain experts propose categorisation into four distinct types, delineated by their predominant symptomatic profiles. The different types of BPD include:
Discouraged borderline is a subtype of Borderline Personality Disorder characterised by a pervasive pattern of hopelessness, low self-esteem, persistent discouragement, and self-criticism. It involves feelings of sadness, shame, and guilt.
Impulsive borderline behaviour involves substance abuse, self-harm, reckless spending, binge eating, unsafe sex, and rash driving. It hinders stable relationships and coping with daily challenges.
It involves irritability, anger, and impulsivity. People with this subtype may be bitter and quarrelsome and exhibit temper outbursts, difficulty controlling emotions, and chronic boredom.
Self-destructive borderline individuals exhibit self-harm, suicidal thoughts, and emptiness. Intense emotional distress may lead to substance abuse and recklessness, accompanied by chronic feelings of worthlessness and hopelessness.
BPD varies in severity. Therapy (like DBT) and, at times, medication can help manage the symptoms. For accurate diagnosis and effective treatment, seek professional help if facing mental disorders.
Recognising the signs and symptoms is important for understanding and empathising with those affected by this disorder. A formal diagnosis necessitates confronting specific symptoms as listed below:
Individuals frequently experience a profound dread of abandonment, even in situations where the likelihood of it occurring is minimal. This fear can lead to frantic efforts to avoid real or imagined abandonment.
Individuals with this condition often have intense relationships. They might see someone as perfect at one moment and then suddenly switch to devaluing them.
People with BPD often have trouble knowing who they are, leading to frequent changes in their goals and values.
Those affected often act impulsively, engaging in self-destructive behaviours like substance abuse, reckless driving, or binge eating.
Self-harming behaviours (cutting or burning) as a way to cope with emotional pain is also one symptom. Individuals with Borderline Personality Disorder may also be at risk of suicide, experiencing recurring thoughts of self-harm.
Often abrupt mood fluctuations, such as intense anger, fear, anxiety, hatred, sadness, and love acompany this condition.
People with BPD often experience a constant feeling of emptiness and boredom, leading to sadness, a sense of something missing, low self-worth, and self-dislike.
Having trouble managing anger is also a symptom, leading to intense outbursts expressed through temper loss, sarcasm, or physical altercations.
Feeling disconnected and having paranoid thoughts or hallucinations during high-stress times.
There is no exact understanding of the cause of Borderline Personality Disorder. No one’s sure why it happens, but researchers believe it’s a mix of genetic, environmental, and neurological factors contributing to its development. It often runs in families, showing a link you can see in changes in certain brain parts that control emotions.
What happens to you when you’re a kid can shape who you become. Bad experiences like being hurt, ignored, or sexually abused, can lead to this condition.
Understanding the intricate links between genetics, brain function, and early-life experiences is important for addressing BPD. This understanding informs targeted interventions, but further exploration is needed to enhance insights and improve management and treatment.
Several risk factors increase the likelihood of developing Borderline Personality Disorder. These factors collectively contribute to the complex origin of the disorder. However, they do not guarantee the development of BPD but rather raise the risk.
These factors include:
Those with a family history of Borderline Personality Disorder (BPD) have a higher risk of developing the disorder.
Differences in the brain’s structure can influence how individuals regulate their emotions and manage impulsivity.
Adverse experiences such as abuse in childhood, neglect, or abandonment increase the likelihood of developing this condition.
Cultural factors, including the interpretation of facial expressions and access to resources, may help develop BPD.
Economic challenges, such as poverty and family disruptions, like parental separation, are social factors that contribute to the risk of Borderline Personality Disorder.
It can have a significant impact on various aspects of a meaningful life.
The major effects include:
People with Borderline Personality Disorder face challenges in relationships due to intense fear of abandonment, mood swings, and impulsivity, leading to frequent arguments and emotional turmoil. It also affects self-perception, making it hard to identify a sense of self, goals, or purpose, resulting in confusion and aimlessness.
Difficulties maintaining steady employment due to mood swings and challenges in interpersonal relationships. In social interactions, those with BPD might find it hard to establish boundaries, resulting in intense relationships characterised by frequent conflicts and strained connections. Consequently, this can lead to isolation in both personal and professional spheres of life.
Overall, dealing with BPD can have a big impact on how you relate to others, see yourself, and feel in general. People facing this disorder need to reach out for the right kind of help and support. It can make a real difference in handling these challenges and improving life.
It requires a thorough assessment by a mental health expert: a psychiatrist or a psychologist. This can be complex because some symptoms often overlap with other mental disorders. However, a careful evaluation will result in an accurate diagnosis and effective treatment planning. Early involvement and treatment can greatly enrich the outlook for individuals with BPD. The process involves:
Let us look at the two major involvements for diagnosing borderline personality disorder:
BPD is diagnosed based on DSM-5 criteria, indicating a pattern of instability in relationships, self-image, and affect. The DSM-5, from the American Psychiatric Association, guides clinicians in consistent and reliable mental health assessments.
A comprehensive psychiatric evaluation diagnoses it by recognising patterns of impulsivity, self-harm, and emotional instability while ruling out other disorders. A holistic approach, combining clinical assessments and collateral information, ensures accurate identification.
When diagnosing, a health provider or therapist examines other mental health conditions similar to BPD symptoms. The conditions include bipolar disorder, histrionic personality disorder, and narcissistic personality disorder. It helps in finding the right treatment.
It often coexists with other mental health disorders, making diagnosis challenging. Conditions include anxiety disorders, bipolar disorders, depression, eating disorders, post-traumatic stress disorders, and substance use disorders.
Effective treatment involves personalised, holistic strategies to address emotional and behavioural aspects, improving life quality. Collaboration with mental health professionals and support networks is important for lasting recovery. Here are some of the common approaches:
Getting therapy is important if you’re dealing with Borderline Personality Disorder (BPD). Different types of treatment include:
DBT promotes mindfulness, emotional regulation, and effective coping, reducing extreme mood fluctuations and enhancing relationships.
CBT targets negative thoughts and actions, addressing inaccurate core beliefs like fear of abandonment to reduce emotional dysregulation and improve patterns of instability in relationships.
Schema Focused Therapy helps individuals with Borderline Personality Disorder identify and change negative beliefs and behaviour patterns for improved well-being.
MBT helps enhance self-awareness and empathy, especially for those with BPD, building stronger connections and improved emotional management skills.
STEPPS, tailored for individuals with this disorder, integrates emotion education, skill development, and support to enhance emotional understanding, problem-solving, and coping.
TFP is about understanding how relationships work and how our past experiences can affect our feelings in current relationships. It’s a way for people with BPD to learn how to build better, more positive connections with others.
While there isn’t a cure for Borderline Personality Disorder, taking medication is an important way to handle issues like feeling down, anxious moments, and acting on impulses. Psychiatrists may prescribe antidepressants for neurotransmitter regulation, mood stabilisers for emotional control, and antipsychotics to address distorted thinking, enhancing overall quality of life.
Getting help early on is essential. Learning about this condition, spreading awareness, and using specific approaches to identify and tackle the symptoms from the beginning is important. Providing information and running awareness campaigns can help identify people at risk early on. By providing targeted support, we can better manage symptoms and encourage a proactive approach to caring for those with BPD.
Early intervention is important for addressing Borderline Personality Disorder. Learn about it, raise awareness, and employ specific strategies to identify and manage symptoms. Spreading information and awareness can help identify at-risk individuals sooner. Targeted support enhances symptom management and promotes a proactive approach..
Untreated (BPD) can show up in different ways, with some common signs like:
Let us explore some special considerations of borderline personality disorder:
Educational programs and awareness campaigns play an important role in reducing the stigma surrounding mental health. They promote open conversations about BPD, helping individuals seek help early on.
Not everyone with this disorder shows the usual signs of the disorder. Some might experience a less intense version of it, while others might have ‘silent BPD,’ suppressing their feelings.
This can be tough, but creating a safe and supportive environment is vital. It’s important to actively listen to their needs, acknowledge and validate their emotions, and encourage them to seek professional help.
Living with BPD involves intense emotions, unstable relationships, and a shifting sense of self. Here are some ways the affected person can seek support and cope with their disorder:
Seeking professional help is important for managing BPD. Medical experts can diagnose, create personalised plans, and teach coping skills, offering vital support for long-term well-being.
Self-help strategies and lifestyle adjustments can be very helpful in managing borderline personality disorder. These strategies and adjustments include:
It is essential to develop a crisis plan for those with borderline personality disorder. The plan may include personalised coping strategies, emergency contacts, and trigger identification, a proactive tool for effective mental health management.
Establishing and engaging with support networks, including friends, family, support groups, or online communities, can provide a vital sense of belonging and understanding.
Borderline Personality Disorder (BPD) faces challenges due to misconceptions and stigma, hindering individuals from seeking help. Addressing these misconceptions is important to promoting understanding, acceptance, and support.
People often misunderstand borderline personality disorder as manipulative or attention-seeking, but individuals with this disorder primarily struggle with painful emotions and relationships. Recognising the real challenges faced by individuals with BPD is important. Therapy, support, and self-care offer the potential for improvement. Challenging misconceptions through open conversations, accurate information, and awareness can reduce stigma.
This is a complex mental health condition that affects approximately 1-2% of the general population. While there has been much progress in understanding the symptoms and treatment, there is still much to learn about this condition. Let us look at some aspects of the current research and future trends of BPD in brief:
Current research aims to uncover the causes and enhance treatments. Scientists investigate neurobiological, genetic, and psychological factors, as well as the impact of childhood trauma, using neuroimaging to study the disorder’s progression.
Exploring borderline personality disorder is becoming fascinating as medical professionals develop personalised treatments and incorporate new technology for enhanced diagnostics and therapy. This innovative approach promises to usher in a new era of comprehending and managing the disorder.

If you’re fighting with BPD, you’re not alone; Psychology Blossom, a Therapy and Counselling Centre based in Singapore, is here to support you. We help you find a supportive haven for your mental health journey. Our dedicated team use easy-to-understand info and chat with you to figure out what works best for you in a super caring way. Psychology Blossom’s psychologists are trained in Cognitive Behavioural Therapy (CBT) and can help guide and regulate your emotions healthily. To book an appointment with us, contact us at +65 8800 0554.
It’s important to remember that borderline personality disorder (BPD) is a mental health condition. As with all mental health conditions, timely intervention can help decrease the disruptions to life. In the journey of BPD, the message is clear: with support, treatment, and a commitment to mental health, a brighter life is within reach.
Seeking support for Borderline Personality Disorder (BPD)?
Contact us for helpful insights and start your journey to healing and resilience!
To learn more, refer to the image below (Suendermann, 2019) or watch the video attached:
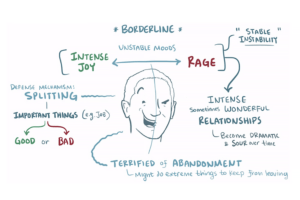
Image Credits: Suendermann, 2019
The symptoms can fluctuate; they don’t usually worsen with age. While treatment and therapy can help manage symptoms at any stage of life, non-intervention may exacerbate the symptoms.
It affects around 1-2 % of the population, more commonly in women. It usually emerges in late adolescence or early adulthood.
BDP is a long-term condition that can improve with treatment like therapy and medication. While it may not completely go away, many individuals experience significant improvements in their quality of life over time.
There is no known cure for borderline personality disorder. However, we can effectively manage it with a combination of psychotherapy, medication, and support from mental health professionals.
People with BPD are not inherently bad. They are fighting with a mental health condition that affects their emotions and behaviour. With treatment, they can manage symptoms and lead fulfilling lives.
The exact cause of BPD is unknown, but a combination of genetic predisposition, adverse childhood experiences, and neurobiological factors likely contribute to its development.
Triggers may include:
Interpersonal conflicts
Stress
Abandonment or rejection
Criticism or perceived criticism
Environmental factors, such as significant life changes
The three common symptoms are:
Distorted self-image
Intense and unstable relationships
Emotional instability
Calming a person with BPD requires validating their emotions, maintaining a calm demeanour, listening actively, avoiding judgement or criticism, and gently encouraging self-care. Setting clear boundaries and suggesting professional help like therapy is also beneficial.